Africa-Press – Gambia. KATHMANDU
On July 23, the World Health Organisation (WHO) declared the recent monkeypox outbreak a public health emergency of global concern.
As of July 27, more than 18,000 cases of monkeypox have been reported to WHO from 78 countries, along with five deaths. Though Nepal has not reported any case of monkeypox to date, health experts say the country needs to be prepared to deal with it as it might be seen in the country at any time because of the open border it shares with India as well as people travelling to Nepal from monkeypox-infected countries. They also advise the need for stepping up surveillance measures at international airports and borders while also making the community aware and informing people about it so that they are ready to deal with it.
A zoonosis
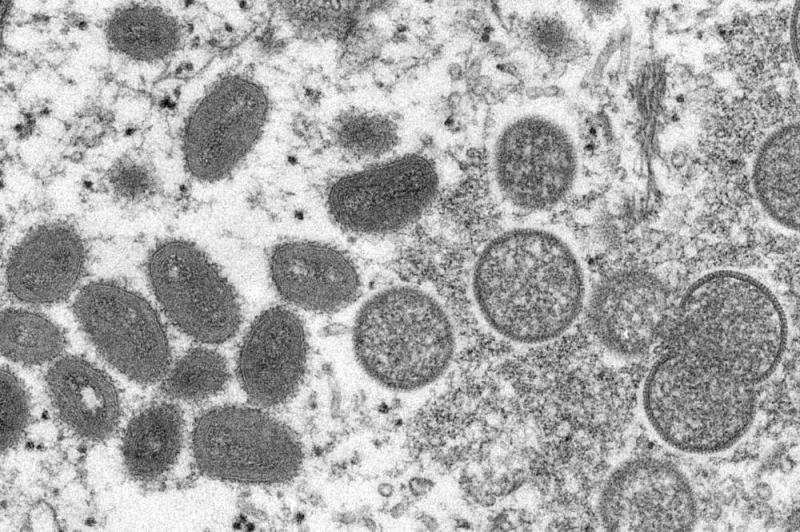
Monkeypox virus is an orthopoxvirus that causes a disease with symptoms similar, but less severe, to smallpox, states the WHO. It is a zoonosis – a disease that is transmitted from animals to humans.
Evidence of monkeypox virus infection has been found in animals including squirrels, Gambian poached rats, dormice, different species of monkeys, and others.
It originated in Africa and spread to the rest of the world, informed Dr Janak Koirala, Professor of Infectious Disease at Patan Academy of Health Sciences, Patan.
Human monkeypox was first identified in humans in 1970 in the Democratic Republic of the Congo while the first monkeypox outbreak outside of Africa was in the USA in 2003. It was linked to contact with infected pet prairie dogs, according to the WHO.
Getting infected
The direct contact with blood, body fluids and mucosal lesions of infected animals can lead to animal-to-human transmission of monkeypox, informed Dr Suravi Pandey, a medical doctor of Internal Medicine at HAMS Hospital, Dhumbarahi.
In the case of human-to-human transmission, she informed, “It can be from skin lesions of an infected person and close contact with respiratory secretions.”
Dr Koirala, who is a member of the Center for American Medical Specialists (CAMS) and works as a Research Consultant at Nepal Health Research Council, added, “The main reason for the spread of monkeypox is skin-to-skin contact between people.”
Such contact between infected and non-infected people has become possible because of globalisation which has led to more frequent “travel, transportation and tourist activities”.
According to Dr Koirala, the gay communities in Western countries have been found to be highly affected by this virus. A July 18 report of the WHO also states that some cases have been identified through sexual health clinics in communities of gay, bisexual and other men who have sex with men, but it is important to note that the risk of monkeypox is not limited to men who have sex with men.
Nonetheless, the monkeypox virus is less contagious than the COVID-19 virus, as per Dr Pandey because “the virus of monkeypox doesn’t remain in the air and the chance of transmission from air droplets is very less”.
She also informed, “The RO (rate of transmission per one infected person to another) value of monkeypox is less than one whereas it is eight for Omicron variant of COVID-19.”
Dr Koirala compared monkeypox’s contagious nature to that of oral herpes and said, “It is transmitted only through close contact and transmission through the air is very less in case of monkeypox.”
What does it feel like when one gets infected with monkeypox? Dr Sanju Babu Shrestha, Head of the Department of Dermatology and Venerology at Nepal Mediciti Hospital, Nakkhu elaborated, “There are rashes on the body and the entire body aches. In the field of dermatology, the symptoms of monkeypox are comparable and are much more similar to the symptoms of chickenpox.
However, it is a relief that it is not as highly contagious as chickenpox.”
Elaborating more on the symptoms of monkeypox, Dr Pandey said, “The interval from infection to onset of symptoms is from six to 13 days and symptoms can continue from five to 21 days.
The minor symptoms include fever, intense headache, swelling of the lymph nodes, and muscle aches. The major symptoms include rashes on the face, palms, soles, inside of the mouth, genitalia and eyes.”
“In 95 per cent of those cases, rashes first appear on the face whereas, in 75 per cent of the cases, rashes start on the palms and soles,” she shared data from the WHO and mentioned that these rashes are pus-filled blisters that crust over and fall off.
Risk for Nepal
The lower RO value than COVID-19 doesn’t mean that it is not an issue of concern.
“As it has already affected many countries in the world, it is a possible threat for Nepal too,” Dr Pandey warned.
Dr Shrestha pointed out the case of India where four people have already been diagnosed with monkeypox.
“This (diagnosis of the monkeypox in India) is a matter of concern for Nepal,” he said while pointing to the open border the two countries share which increases the chance of the infection entering Nepal at any time.
“As it is more infectious in crowds, people travelling via public vehicles and exposed to public areas must be cautious in Nepal,” he cautioned.
“If the cases rise in the world and mainly in India, then it will definitely enter Nepal. My estimation is that 10 to 20 people will be infected initially and the infection can rise to 100 to 200 people at the maximum in the first period (wave) of monkeypox infection in Nepal. However, if both the government and public fail to take preventive measures and manage the situation, then it may get more contagious,” Dr Koirala warned.
The doctor also sees higher chances of the spread of monkeypox infection in Nepal as it is a country where people live in joint families. “Nepalis have a culture of sharing utensils, clothes, bed sheets, and towels.
So, if a member of a family is infected, all members will be infected,” he said.
The other areas with crowds like schools and colleges are also at risk as students can get infected by their classmates and can transmit the virus to their family members, he shared.
Symptomatic management
What can be done when a person gets infected? “There is only symptomatic management of monkeypox.
The symptomatic people must be given paracetamol to reduce fever and pain. One should drink lots of water and eat proper nutritional food.
Monkeypox subsides in two to four weeks. However, if a patient’s immunity is low, they can develop pneumonia, infection of the brain, sepsis and eventually die. The mortality rate is three to six per cent,” Dr Pandey informed.
Dr Koirala called monkey-pox a self-limited disease (a person is cured on his/her own because of immunity, without specific treatment) that does not have a high mortality rate. “However, if the person has low immunity power, then it can result in death,” he said.
One of the ways to prevent the infection is vaccination against monkeypox, like in the case of COVID-19, as per the health experts.
“There is a vaccine known as vaccinia virus for Ankara strain (of chickenpox) and was approved for the prevention of monkeypox in 2019.
This is a two-dose vaccine,” said Dr Pandey sharing WHO information regarding the vaccine against monkeypox.
She clarified that there is no vaccine specifically for monkeypox as of now “but the vaccine against smallpox has been seen effective in the prevention of monkeypox infection”.
Dr Shrestha added to that, “Thus, antibiotics and paracetamol are the only medicines that can be given to reduce pain. The exposure of healthy people must be minimum with people suspected of being infected with monkeypox – one has to maintain physical distance and wear a mask and use hand sanitiser. We have learned many things from COVID-19 – the same safety measures can be applied in this case too.”
Meanwhile, Dr Koirala shared, “The WHO and Nepal Health Research Council have proposed to do trial to find out which medicines are effective to treat monkeypox and also to make its vaccine.”
Staying safe
Cases of monkeypox have not been reported in the country as of now though it has been spreading across the globe. In such a situation, the experts say the virus will one day enter Nepal.
What can we do at an individual level to prevent getting infected? Dr Koirala said, “Wearing full-sleeved clothes is one of the ways to prevent transmission in public transportation.
Since only close skin-to-skin contact with an infected person is needed for the virus to infect a healthy person, covering the body with clothes can be helpful to prevent it to an extent. But people should maintain social distance when in a crowd.”
Dr Pandey suggested, “Any kind of meat must be cooked well before eating. The infected should wear a mask, gloves and face shield. The items used by monkeypox patients must be cleaned separately. A healthy person should also always wear a mask, use a sanitiser, and wash hands from time to time.”
But if a person has some kind of skin problem, s/he should visit a hospital. “In case an individual is diagnosed with monkeypox, the patient will have to stay in the infectious diseases hospital for three weeks. Healthcare workers must be equally cautious.
The hospital employees must wear gloves. In the case of monkeypox, hand sanitiser is more efficient than hand washing. As it is not as infectious as COVID-19, there is no need for special equipment and isolation like in the case of COVID-19, only no physical contact with the infected person is sufficient to be safe from monkeypox,” Dr Koirala suggested.
But efforts are needed at the community and the government’s level too, as per the doctor, who recommended, “Prevention is better than cure. Awareness is lacking and especially needed in Nepal about monkeypox. The people who are coming from abroad should be made aware to maintain a safe distance in the community so that if they are infected they do not transfer it to the community. And, also the community must be cautioned on how we should maintain a safe distance from people coming from abroad and remain safe. Awareness campaigns must be done, especially in remote areas of Nepal, as well as in crowded places like schools. There is no need to panic but awareness is important. The government had done awareness campaigns at some level but that is not sufficient.”
Dr Shrestha meanwhile pointed to the risk of the open border and said, “The surveillance at the border and airports must be done properly.”
Dr Pandey also emphasised the need for “strict surveillance at airports and border areas. Proper screening of patients with fever and rashes should be done and reported,” she said.
Dr Koirala added, “The border and international airport of Nepal must be tightly checked as people coming from abroad carry the risk. The government must screen people coming from abroad and tourists. The government has put COVID-19 health desks at the international airport and border check posts. Now, it must add health desks for monkeypox, too.”
He also urged the government to focus on vaccination in consultation with the WHO.
In case a person is diagnosed with monkeypox in Nepal, “isolation and vaccination of the patient is a must,” Dr Shrestha said.
Dr Koirala echoed a similar view, “The government must be ready with contact tracing and quarantine policies in case monkeypox cases are seen in Nepal.”
A version of this article appears in the print on July 31, 2022, of The Himalayan Times.
For More News And Analysis About Gambia Follow Africa-Press