DR DAVID KARIUKI
Africa-Press – Kenya. In Kenya healthcare disparities often mirror the gaps between urban affluence and rural neglect, therefore the gazetting of the Medical Practitioners and Dentists (Medical Institutions) (Amendment) Rules on December 31, 2021, felt like a quiet revolution that prioritised patient safety over bureaucratic inertia.
As we mark nearly four years since these rules came into effect, it’s worth reflecting on their intent and impact. Far from being just another layer of red tape, these amendments represent a bold recalibration of Kenya’s health system, aligning it more closely with the realities of our diverse needs.
But while they offer a blueprint for progress, their true success hinges on rigorous enforcement and stakeholder buy-in. These rules primarily revise the previous classification system (The Medical Practitioners and Dentists (Medical Institutions) (Amendment) Rules, 2017) to better align services with facility capabilities.
The core amendment involved deleting the old classification and substituting with a new one, expanding the system to 12 levels modelled in line with the Kenya Essential Packages for Health.
This change reflects evolving healthcare needs, emphasising preventive care at community levels and ensuring higher levels handle complex services only with available resources.
Prior to 2021, Kenya’s health facilities were broadly categorised into about seven levels, with the basic unit often a clinic (level 2 or 3) that could vary widely in quality.
This led to inconsistencies, where under-equipped facilities might attempt to provide advanced services. The 2021 amendments introduce finer distinctions, incorporating community-level units and sub-levels to better reflect actual capabilities.
The primary objectives of this reform were to enhance patient safety by ensuring that services offered are strictly commensurate with the facility’s approved level and capability.
Secondly, to eliminate the previous practice where facilities of widely varying capacity were lumped together under broad categories (especially at level 2), which encouraged over-reaching and compromised quality. Third, to facilitate evidence-based planning, equitable resource allocation and effective referral systems across the country.
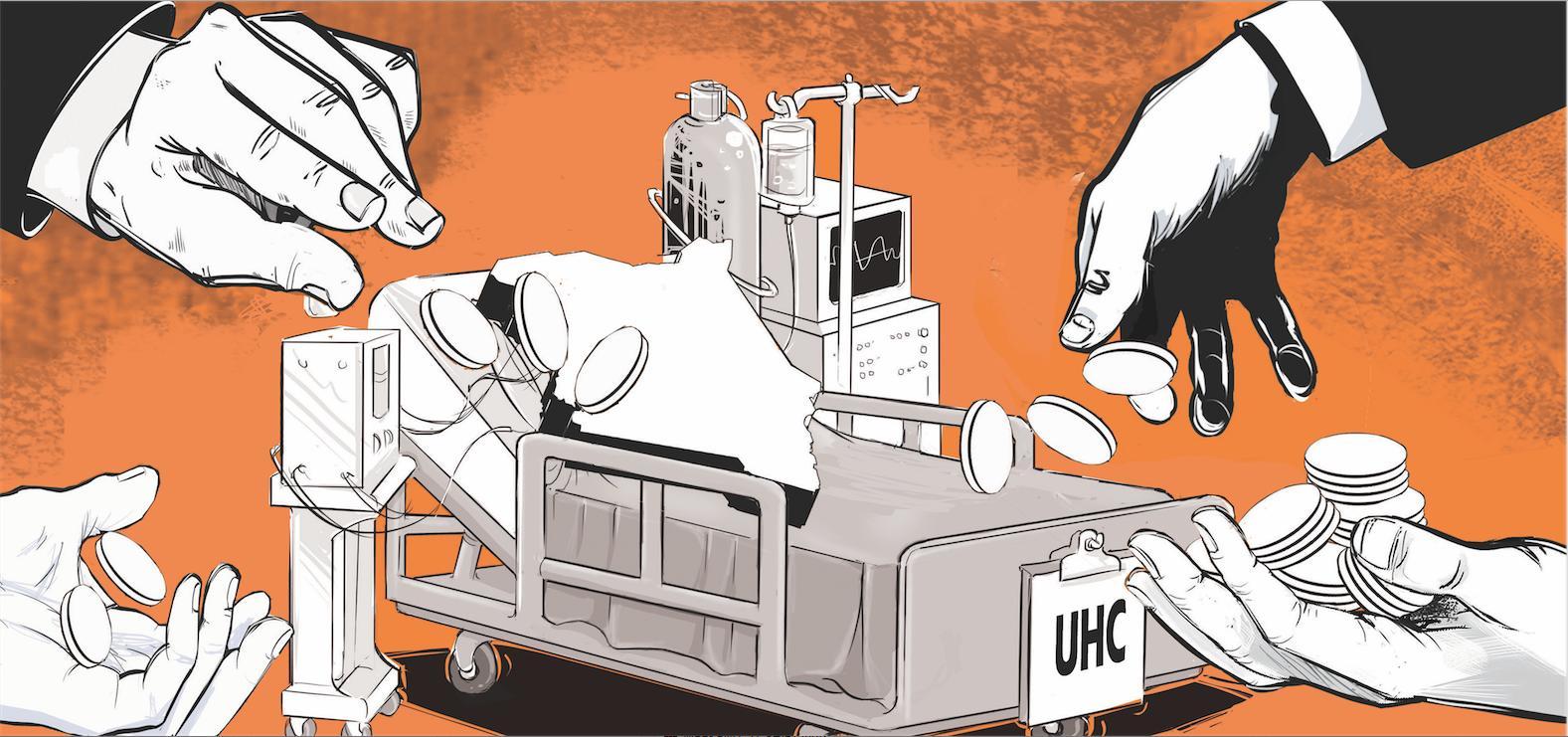
The objectives also aimed to support Kenya’s universal health coverage (UHC) agenda by clearly defining the role of each level in preventive, promotive, curative and rehabilitative care and empower members of the public to make informed decisions about where to seek appropriate care for their needs.
It is important to note that the 2021 rules introduced a 12-level categorisation of health institutions up from the previous seven levels for more granular regulation based on service capacity, human resources and infrastructure.
The rules additionally shift the basic unit to the community health unit, focusing on preventive and promotive care, including early screening, sets facilities run by medical or dental practitioners at Level 3B (general medical or dental practice clinics) as the entry point for doctor-led care, aim to prevent facilities from offering services beyond their capacity, improve quality control, and help the public identify appropriate care levels.
Other effects of the rules are higher levels (4–6) are reserved for comprehensive primary, county and referral hospitals with defined minimum requirements for infrastructure, staffing, diagnostics, theatre capacity and specialised services.
Level 6 facilities were split into level 6A and 6B to better reflect varying capacities among national referral hospitals. The rules address gaps in the older system, where clinics could operate at level 2 regardless of capacity.
The updated structure ensures services match infrastructural and staffing quality. The guidelines benefit the public by clarifying service expectations for specific services at each facility level.
The rules were also published on the council’s website. Health facilities and practitioners should continue to familiarise themselves with the rules as the council expects compliance during inspections and licensing.
The categorisation supports Kenya’s broader health policy goals, such as UHC, by promoting appropriate referrals and resource allocation. The implementation is gradual and continuous as health facility verification is undertaken.
The council remains committed to supporting health facilities through this transition and encourages prompt action to ensure continued compliance and improved quality of care for all Kenyans. CEO, Kenya Medical Practitioners and Dentists Council
Source: The Star