Africa-Press – Rwanda. For many centuries, before the emergence of modern pharmaceuticals, Rwandans relied on traditional medicine and therapies to cure diseases.
Traditional medicine was an integral part of Rwandan culture since time immemorial, serving as a primary source of healthcare for many, especially in rural communities.
Today, several studies have shown that despite advances in modern medicine, more Rwandans are turning back to traditional healing practices, using herbal medicine alongside modern treatments in response to the declining efficacy of some industry-made drugs and increasing resistance.
For people like Alphonsine Mukeshimana, traditional Rwandan medicine is effective and can play a vital role in treating diseases, especially if it is modernised and packaged in a way that makes it accessible to many.
Mukeshimana says that for many years, she struggled with uterine fibroids, which doctors often treated with surgery, only for them to recur. However, one day, she met an elderly woman who offered her traditional herbal medicine, claiming it would heal her for good.
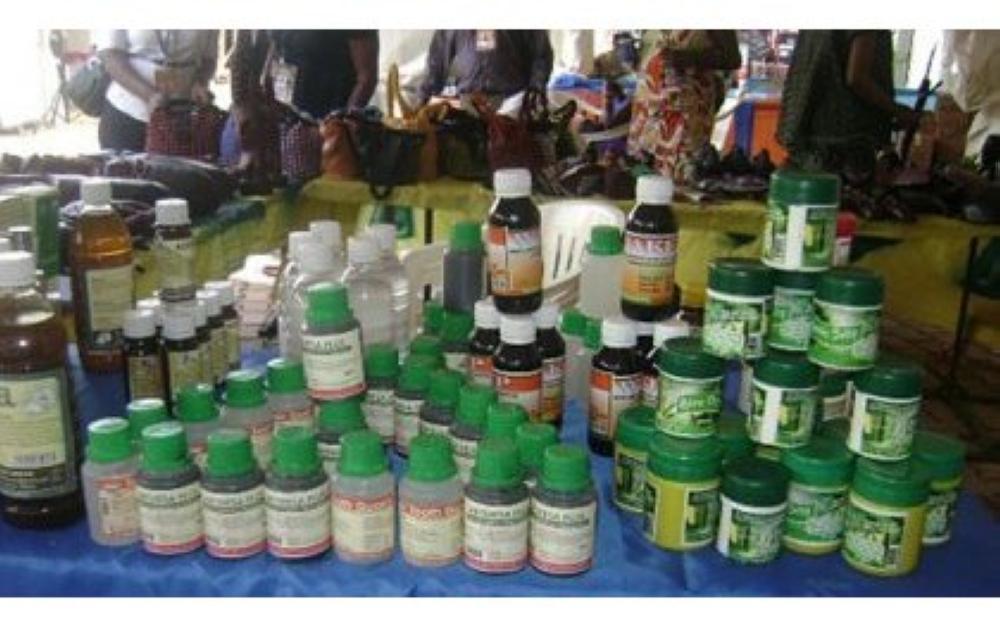
Some of traditional medicines showcased during the exhibition_
“I had always doubted the efficacy of traditional medicine, but after taking the herbal treatment for two months, my uterine walls cleared. I kept doing scans, and there was no recurrence,” says Mukeshimana, who has since become an advocate of traditional medicine.
With the recurring fibroids, doctors had warned her that she could develop cancer, which scared her deeply. She embarked on a journey of using traditional therapies and eating organic, nutrient-rich foods and fruits.
Today, Mukeshimana says she has never been healthier, thanks to the herbs and food choices, which she notes are low-cost or even free since most of the ingredients can be found in nature or purchased affordably in the market.
“We have all these medicinal trees and plants around us, but it is unfortunate that we don’t realise their value until we fall sick. The healthiest foods, like vegetables, are the least expensive, and most of the herbs can be obtained for free in our surroundings,” she says.
Mukeshimana believes that if Rwandans could return to practicing some traditional healing methods, with a degree of regulation, it could help reduce the burden of non-communicable diseases in the country.
While Rwanda has made great strides in improving access to conventional healthcare through numerous health posts, health centers, and district and referral hospitals, more Rwandans are now adopting traditional methods to treat or prevent certain diseases.
The Rwandan government recognises the significance of traditional medicine and has been working towards integrating it into the national healthcare system, but there is still much work to be done.
However, traditional medicine remains highly regulated due to challenges in the industry, where certain beliefs and practices have been mixed with therapies, sometimes leading to manipulation, deception, or misinformation that prevents people from seeking proper treatment.
Despite these challenges, Daniel Gafaranga, a traditional healer and former president of the Rwanda Network of Traditional Healers, locally known as Abavuzi Gakondo, believes that with proper regulation and incentives, traditional medicine can help Rwanda significantly reduce its disease burden.
Gafaranga blames what he calls ‘charlatans’ who infiltrated the traditional medicine industry, tarnishing its credibility through dubious practices and rituals that are not genuinely related to traditional medicine.
“I can say the traditional medicine sector still faces many challenges. I identified these issues during my eight-year tenure as president of the network,” he says, adding that in March 2011, when the government called for the regulation of traditional medicine, the majority of those who registered were not genuine traditional healers.
“We had people who could be classified as ‘spiritual healers,’ locally known as Abarangi, who perform certain rituals while practicing traditional medicine, including playing drums and reciting certain words. They made up 60 per cent of the registrants.”
Another 20 percent were ‘bone-setters,’ commonly known as Abagorozi, while traditional healers who met all the requirements comprised just 10 per cent.
The remaining 10 per cent were soothsayers and magicians who claimed to ‘perform miracles’ and used this to deceive unsuspecting Rwandans.
Gafaranga attributes the slow development of the traditional medicine sector to these imposters, who joined the field seeking financial gain rather than offering real solutions.
He says they use objects such as animal skins and charms to convince people while lacking true knowledge of traditional medicine.
“These are people who saw it as an opportunity to make money rather than to heal. If you were to go around Kigali today and identify ten genuine traditional healers, you wouldn’t find them because of this issue,” he says, adding that such individuals have made it difficult for authentic traditional medicine practitioners to operate.
“I hope the Ministry of Health will develop a plan to support traditional medicine, but currently, only 10 percent of us are recognised and work with institutions such as INES Ruhengeri and NIRDA to advance the field,” he says.
Moving traditional medicine to MINUBUMWE
Gafaranga argues that for traditional Rwandan medicine to take root, it should be moved to the Ministry in charge of Unity and Culture, which is tasked with preserving Rwandan culture and traditions.
“I believe traditional medicine would thrive if it was moved to the Ministry of National Unity and Civic Engagement, allowing it to develop quickly because there is a connection between traditional medicine and culture,” he argues.
“Traditional medicine is currently under the Ministry of Health, which follows strict procedures. They want something that has been tested, examined, and confirmed by research,” he adds.
However, he asserts that traditional medicine is more rooted in cultural practices passed down by ancestors to treat diseases, including those that modern medicine has struggled to cure.
For this reason, he believes traditional medicine should be transferred to MINUBUMWE, as it is deeply linked to culture and its practices. This move, he says, would allow it to develop and complement conventional healthcare more effectively.
A rich heritage
Gafaranga states that Rwanda has a vast catalogue of traditional medicines that, if well developed, could treat many conditions, including gastrointestinal diseases, liver and heart diseases, and skin ailments.
“We have medicine derived from traditional herbs that can cure ulcers, poisoning, papilloma wounds that are not cancerous, and many other diseases. Each condition has a corresponding herbal remedy, and these have been proven highly effective,” he explains.
“Although we have dermatologists who treat skin diseases, we also have traditional herbal medicine that treats skin conditions effectively,” says Gafaranga.
Among key herbal medicines, he mentions ‘Inyabarasanyi’ or the ‘Blackjack’ weed (Bidens pilosa), which he claims is highly effective in treating fresh wounds and injuries.
“Our ancestors named it ‘Inyabarasanyi’ because warriors used it to heal their wounds during wartime. This herb not only heals wounds effectively but also promotes blood flow,” he says.
Another essential herb he highlights is “Ikirigora,” known as “African Ginger,” which was traditionally used to relieve pain while identifying underlying health problems.
Gafaranga also emphasizes the significance of Vernonia amygdalina, known locally as ‘Umubirizi,’ which has been widely used to treat diabetes, hepatitis B and C, stomach ailments, and more.
“It is one of the most powerful medicinal plants in Rwanda. It benefits diabetic patients, people with hepatitis, and those suffering from stomach issues,” he says.
For mental illnesses, he mentions ‘Umusendabazimu’ (Withania somnifera), which he claims has high efficacy in treating conditions related to the mind.
“If this plant were integrated into conventional treatments, it could play a key role in preventing mental conditions,” he says.
He also references ‘Artemisia,’ which has been used for centuries to treat malaria. Though its commercial cultivation began only recently, Rwandans traditionally used it for both treatment and prevention.
“It is a miraculous plant. Even during the COVID-19 pandemic, it was used to treat symptoms. The Ministry of Health acknowledges its efficacy,” he notes.
Other notable herbs include ‘Magaru’ (Hypoestes triflora), used for liver and gut conditions; ‘Igisura’ (Urtica massaica), a lactogenic plant that promotes breast milk production; and many more, such as ‘Umukoni’ (Synadenium grantii), ‘Umuravumba’ (Tetradenia riparia), and ‘Igicuncu’ (Plectranthus barbatus).
Addressing challenges of dosage and allergic reactions
Gafaranga acknowledges that, like modern pharmaceuticals, some individuals may be allergic to herbal medicine, a reaction traditionally known as ‘Ubwivumbure.’
“If a person experiences a reaction, we advise them to eat uncooked food, such as a banana or raw carrot, before consuming cooked food. This helps mitigate the reaction,” he explains.
Traditional medicine also has established dosage guidelines. He says that Rwandans historically took medicine in its concentrated form, consuming only a few mouthfuls equivalent to two spoonfuls or sips, ensuring effectiveness.
However, he warns against quack healers who dilute herbal medicine, reducing its efficacy.
In terms of safety, traditional medicine relied on animals to determine plant safety.
“If a plant is safe for animals like goats and cows, it is also safe for human consumption. This has been the standard method used by traditional healers for centuries,” he says.
Challenges in traditional healing practices
Gafaranga highlights a critical issue: some unqualified traditional healers fail to inform patients about life-threatening conditions, delaying proper treatment until it is too late.
“It is crucial for traditional healers to be honest and refer patients to hospitals if their condition requires advanced medical intervention. False promises can cost lives,” he warns.
He also criticizes the sale of traditional medicine in unhygienic conditions by street vendors, which compromises quality and fosters mistrust.
“My advice to Rwandans is to avoid purchasing medicine from unverified sources. Instead, they should seek treatment from recognized traditional healers with proper premises,” he says.
Investing in research
Marc D’Haenen, a phytotherapist based in Rwanda, has spent the last eight years researching how Rwandan medicinal plants can be integrated into mainstream healthcare.
Working with the Nyirinkwaya Foundation, established by Dr. Jean Nyirinkwaya, D’Haenen has focused on medicinal plants, natural remedies, and organic pesticides, drawing inspiration from Rwandan traditional medicine.
“Rwandans have used traditional medicine for centuries, and it remains relevant today. There is a need to upgrade these practices, not to replace them but to evolve them for better effectiveness,” says D’Haenen, the foundation’s Executive Secretary.
On a large farm in Bugesera, he and Dr. Nyirinkwaya are developing synergetic farming systems based on crop diversity, resilience, and sustainability.
Their goal is to create a fully-fledged research and agricultural center where people can learn about Rwanda’s traditional healing practices.
“Each day, we deepen our understanding of Rwandan medicinal plants,” he says, emphasising the need for further research to integrate traditional medicine into mainstream healthcare.
Regulating traditional medicine
The Rwandan Ministry of Health has taken steps to regulate traditional medicine through the National Policy of Traditional, Complementary, and Alternative Medicines, released in February 2019. The policy outlines measures for registering and monitoring traditional healers to ensure safety and prevent malpractice.
Various collaborations between universities and medical researchers have focused on studying the efficacy of herbal treatments and educating the public on the safe use of traditional medicine.
However, challenges such as lack of standardisation, value addition, and limited scientific research continue to undermine credibility and trust in traditional medicine.
Despite these obstacles, traditional medicine remains an essential part of Rwanda’s healthcare system, offering accessible and culturally relevant treatment for many.
With the right policies, investment in research, and regulation, it can effectively complement modern medicine and contribute to national healthcare goals.
For More News And Analysis About Rwanda Follow Africa-Press